AUTONOMOUS/CLOSED LOOP CONTROL FOR COMBAT CASUALTY CARE
KEY BENEFITS
- “First of its kind” Food and Drug Administration investigational device exemption (IDE) clinical trial for automated oxygen control
- Optimizes care for patients requiring mechanical ventilation, particularly during large-scale combat operations or prolonged casualty care
- Optimal oxygen delivery, oxygen supply savings/reduced requirements, improved patient management during patient movement
WHAT IS IT?
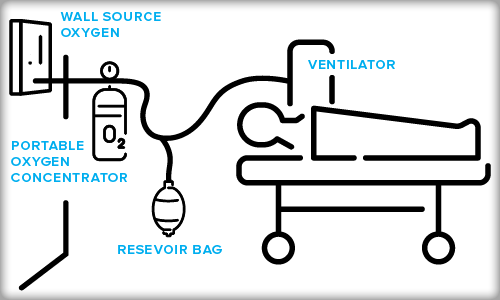
Providing care for combat casualties often requires the use of mechanical ventilation (MV) to provide accurate oxygen delivery and support safe, efficacious patient care during movement across expeditionary and en route care (ERC).
The use of mechanical ventilation requires adjustments to ventilator settings unique to each patient managed by clinicans to ensure proper oxygenation levels.
This technology automates the adjustments for ventilatory support by advanced monitoring to maintain proper oxygenation to clinician-targeted levels.
A secondary attribute of this technology is the ability to utilize a portable oxygen concentrator (POC) which is controlled by the mechanical ventilator.
The operational outcomes of ACLC/MV/POC are optimal oxygen delivery, substantive oxygen supply savings/reduced oxygen requirements, improved patient management and care during patient movement, enhanced quality of care between patients and medical personnel, and efficacious movement across expeditionary and ERC Systems.
HOW DOES IT WORK?
Over the last 10 years, AFRL, in collaboration with the University of Cincinnati, Zoll Medical, and Caire Inc., has researched and developed this technology.
These efforts included a full review of protocols and the development of software for automatic adjustment of oxygenation to maintain the oxygen levels within a target range based on continuous use of pulse oximetry.
The system utilizes an algorithm embedded in the mechanical ventilator designed to increase or decrease the amount of oxygen required to ensure proper oxygen levels for combat casualties.
During the FDA IDE clinical trial, the system made 306 oxygenation automated adjustments in a 12-hour period compared to 10 adjustments made by clinicians.
The ACLC MV enhances combat casualty and patient care and avoids hypoxemia and hyperoxemia and the attendant consequences. The system is a force multiplier with an improved standard of care, reduces clinician time in managing patients, expands medical capacity to care for patients, reduces logistical footprint, and contributes to the future state of autonomous patient movement.
WHY IS IT IMPORTANT?
The future battlespace will include dispersed and multidomain operations within austere environments, congested communications, and advanced weaponry. Such conditions will result in high volumes of wounded, ill, and injured (WII), generating new injury patterns and complicating casualty movement in and out of theater due to enemy advances in anti-access/area denial capabilities. In addition, it increases the level of saturation on combat casualty care clinicians. Our military medical personnel must be able to mitigate the impact of injuries and rapidly maximize the combat effectiveness and survivability of warfighters.
Mitigation must include automous care systems. This technology will decrease task load, act as a force multiplier, and allow for expanded critical care.
This technology will also enhance critical care air transport teams increasing the capability to provide for multiple high-acuity patients simultaneously during patient movement.
ADDITIONAL FACTS
The first spiral development of this technology focused on Fraction of Inspired Oxygen with an alternate oxygen source.
The technology is being evaluated for advanced development efforts to gain FDA approval/clearance.
Further research is being completed for fully closed-loop control of oxygen, minute ventilation and decision assist function positive end expiratory pressure (PEEP).
The goal for ACLC/MV is to develop a closed-loop mechanical ventilation system that will be used jointly by all the services. Currently, some patients are subject to a ventilator change at different roles of care due to differences in the ventilators used across the services, which may result in delays and adversely impact patients. With the closed loop function, patients can be moved through roles of care without changing ventilators or, when changes are necessary, mitigate potential complications, reducing patient harm.